"Age is just a number, not a state of mind or a reason for any type of particular behavior."
-Cecelia Ahern
Alzheimer's disease is the sixth leading cause of death in the U.S., although recent estimates indicate it may now be the third most common cause of death, behind heart disease and cancer, according to the National Institute on Aging.
The Severity Of Alzheimer's
Alzheimer's is the most common cause of dementia, a generic term for memory loss and other cognitive abilities serious enough to interfere with daily life. About 60-80 percent of dementia is traced back to Alzheimer's, according to the Alzheimer's Association.
The NIA defines Alzheimer's as an irreversible, progressive brain disorder that gradually destroys memory and thinking skills and eventually even the ability to perform the simplest of tasks.
The disease takes its name after German psychiatrist Alois Alzheimer, who first discovered the deposition of abnormal proteins in the brain.
With age being the major risk factor for Alzheimer's, the rapidly aging U.S. population could engender 1 million new cases per year by 2050, according to the National Institutes of Health.
Morgan Stanley analyst Matthew Harrison expects the market for Alzheimer's drugs to grow to $300 billion.
The Causes
Alzheimer's is thought to result from a combination of genetic, lifestyle and environmental factors, according to the NIH.
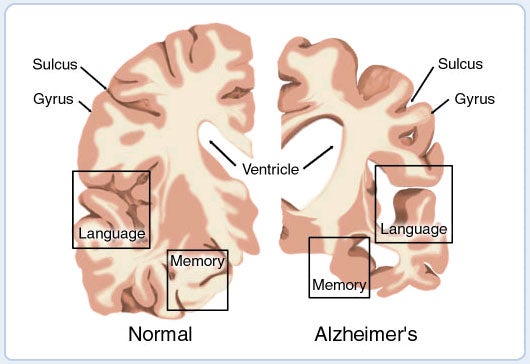
Age-related changes could lead to shrinking of some parts of brain, mainly the cerebral cortex, which is responsible for higher functions such as memory, and processing thought. Clumps of protein called plaques and tangles form in the brain, resulting in the loss of brain cells and in turn reduced neurotransmitter chemicals such as acetylcholine and dopamine, which are responsible for the transfer of nerve impulses from one nerve cell to another.
Source: ZMEScience
Other changes include inflammation, the production of unstable molecules called free radicals and the breakdown of energy production within cells. All of these factors harm nerve cells and contribute to Alzheimer's.
Genetically, the presence of a form of the apoliprotein E — or APOE — gene on chromosome No. 19 increases the risk of Alzheimer's.
Some lifestyle factors that are believed to contribute to Alzheimer's include smoking, high blood pressure in midlife, depression, diabetes and a lack of physical activity, cognitive stimulation and social engagement.
Alzheimer's Treatment
Alzheimer's has no cure, but its symptoms can be treated. Five treatment options are FDA-approved for Alzheimer's symptoms and several more potential products are in the pipeline.
Pfizer Inc. PFE's donepezil, sold under the brand name Aricept, has been on the market since 1996 and belongs to a class of medication called cholinesterase inhibitors. It acts by preventing the breakdown of acetylcholine, a neurotransmitter chemical that's important in the cognitive process.
Novartis AG (ADR) NVS's Exelon or rivastigmine was approved in 2000 for treating mild to moderate dementia caused by Alzheimer's and Parkinson's disease.
Razadyne, chemically galantamine, is used to treat mild-to-moderate Alzheimer's and other memory impairments. It was developed by Johnson & Johnson JNJ.
Memantine, sold under the brand name Namenda, was approved by the FDA in 2003. It was originally developed by Forest Labs, which was later acquired by Actavis. Actavis is now known as Allergan plc Ordinary Shares AGN following its acquisition of the latter company. Namenda is the only FDA-approved drug for treating Alzheimer's that is not an acetyl cholinesterase inhibitor. It acts by blocking the current flow through NMDA receptor-operated ion channels, reducing the effect of excitotoxic glutamate.
A combination drug from Allergan and Adamas Pharmaceuticals Inc ADMS, Namzaric — chemically donepezil and memantine — was approved in 2014.
See also: Attention Biotech Investors: Brace For These January PDUFA Events
Research With Long Odds
Alzheimer's drug development is considered to have the highest failure rates of all drug research, at 99.6 percent compared to 81 percent for cancer, according to Scientific American.
The reasons are obvious. The brain, being inaccessible, is a difficult place to test and administer a drug.
The amyloid hypothesis, the premise for Alzheimer's drug development, is seen by many as unconvincing, given the lack of success found with the approach.
"Our level of ignorance is cripplingly high. This is coupled with the heterogeneous nature of the disease, the difficulty of diagnosing it in the first place — essential for selecting patients in a trial and treating them later — and its very slow progression," the Scientific American said, quoting medicinal chemist and blogger David Lowe.
Amyloid plaques deposit in the brain for about a decade or more before symptoms become apparent. Testing is therefore typically done in patients who have advanced deposits.
"Ideally, scientists must figure out who is most likely to get Alzheimer's — then see if they can prevent healthy brains from developing it," Dr. Mike Hutton, the chief scientific officer for neuroscientific drug discovery at Eli Lilly and Co LLY, was quoted as saying in The Guardian.
Pfizer Exits Alzheimer's Space
Pfizer, among the first companies to research Alzheimer's, announced recently that it would end R&D on new drugs for Alzheimer's and Parkinson's diseases. The logic: the funding can be reallocated to areas where the company has strong scientific leadership, helping to provide the greatest impact to patients.
In 2012, the company had to discontinue the development of bapineuzumab after Phase II trials revealed that the candidate did not adequately benefit patients with mild-to-moderate Alzheimer's.
Axovant's Intepirdine Falls Flat
Axovant Sciences Ltd AXON said Jan. 8 that it plans to discontinue its intepirdine program, based on the results of the MINDSET, HEADWAY and Gait and Balance studies. In late September, the company said its late-stage MINDSET trial of the 5-HT6 inhibitor intepirdine failed to improve the cognition or activities of daily living relative to a placebo in patients with mild-to-moderate Alzheimer's.
Biogen Rests On Hope
Biogen Inc BIIB is persisting with its Alzheimer's candidate aducanumab, dubbed BAN2401, which it is co-developing along with Eisai Co., Ltd (ADR) ESALY. This is despite the company announcing in December that an independent data monitoring committee determined that BAN2401 did not meet the criteria for success based on a Bayesian analysis at 12 months as the primary endpoint in an 856-patient mid-stage trial.
BAN2401 is an anti-amyloid beta protofibril antibody.
The blinded study will continue, with a comprehensive final analysis to be conducted at 18 months, according to Biogen. The companye expects results during the second half of 2018.
Biogen is also developing elenbecestat, dubbed E2609, for which a Phase III trial is underway.
Eli Lilly Forms Development Partnerships
After Eli Lilly's Alzheimer's candidate solanezumab failed to meet the primary endpoint in a late-stage study in 2016, the company forged an alliance with AstraZeneca plc (ADR) AZN to develop an Alzheimer's treatment option, namely MEDI1814, by paying AstraZeneca $30 million upfront. MEDI1814, originally developed by AstraZeneca's biologics arm MedImmune, binds selectively to amyloid beta 42, which is believed to cause plaques.
Eli Lilly and AstraZeneca were already collaborating on a beta secretase cleaving enzyme — or BACE — inhibitor, AZD3293, which was again a rebound attempt by Lilly after its own BACE program in Alzheimer's was shelved due to liver toxicity issues.
AZD3293 was accorded fast track designation status by the FDA in August 2016 and it is in a Phase III trial. The results are expected in 2019.
Merck Stays On Course
In February 2017, an external data monitoring committee warned that Merck & Co., Inc. MRK's Alzheimer's candidate verubecestat faced potential failure in a Phase II/III study, prompting Merck to discontinue the study.
The company went ahead with another late-stage, two-part study, APECS, for people with prodromal Alzheimer's. The results of the study are due in February 2019.
Merck bought an exclusive worldwide license from Japan's Teijin Pharma to develop an investigational, preclinical anti-tau antibody. Tau proteins are aggregates of hyperphosphorylated protein found in a group of diseases called tauopathies, which includes Alzheimer's disease.
Roche's Progress
Roche Holding Ltd. (ADR) RHHBY's Alzheimer's drug crenezumab, an anti-amyloid beta antibody, is in Phase III trials for treating patients with prodromal to mild AD.
Roche faced a setback in 2014 when crenezumab failed to meet the co-primary endpoints of a Phase II trial, where the drug was tested in mild-to-moderate Alzheimer's. Roche decided to push ahead with two Phase III trials, with increased dosing.
Crenezumab was licensed from AC Immune SA ACIU by Roche's Genentech unit in 2006.
Data from the first Phase III trial is due in 2020.
Johnson & Johnson's Renewed Push
Johnson & Johnson recently announced a partnership with the University of Pennsylvania that would combine the former's anti-Alzheimer's antibodies with the latter's adeno-associated viruses, or AAVs. J&J expects to use AAV viral delivery to trigger the expression of therapeutic antibodies in the brain, overcoming the blood-brain barrier.
Novartis, Amgen Collaborate On Preventive Treatment
In November, Novartis and Amgen, Inc. AMGN, along with the Banner Alzheimer's Institute, announced a collaborative new "Generation Study 2" to assess whether the BACE1 inhibitor CNP520 can prevent or delay symptoms of Alzheimer's. The study is to be conducted on cognitively healthy people who are at genetic risk of developing Alzheimer's.
Startups Tackle Alzheimer's Despite Risks
Denali Therapeutics Inc. DNLI's DNL747 is being tested for its effectiveness in diseases that include Alzheimer's. Morgan Stanley said it expects news on target engagement and dose selection in 2018, with key clinical data arriving in 2019.
Another start-up, Verge Genomics, has taken the route of mapping hundreds of genes that are coregulated to cause a disease based on voluminous data from DNA, RNA and protein. This information is used to develop a drug that targets all genes at once.
The Weed-Alzheimer's Connection
Apart from conventional drugs, research shows that therapeutic low doses of THC — tetrahydrocannabinol, the principal psychoactive constituent of cannabis — can bind to the amyloid-beta protein, preventing it from aggregating. This, in turn, can slow the formation of amyloid-beta plaques around neurons.
Related Link:
Analyst: When Americans Sneeze, Teladoc And Athenahealth Profit
© 2025 Benzinga.com. Benzinga does not provide investment advice. All rights reserved.
Trade confidently with insights and alerts from analyst ratings, free reports and breaking news that affects the stocks you care about.